Perineural injection therapy is a gentle new way to use Dextrose to treat painful musculoskeletal conditions by promoting tissue healing and nerve desensitization. Perineural prolotherapy targets painful superficial nerves by injecting low-concentration dextrose (most commonly 5%, D5W) along the nerve’s subcutaneous course. The aim is to calm neurogenic nerve pain or hypersensitivity by providing stimulation to restore normal nociceptor/peptidergic function; it is distinct from classic prolotherapy, which uses higher-concentration dextrose placed into ligaments/tendons to stimulate connective-tissue repair.
A Brief history
- 1940s–1990s: “Prolotherapy” (deep injections of hypertonic dextrose) develops as a soft-tissue regenerative approach (Hackett, et al.).
- 2000s: John Lyftogt popularizes perineural (superficial) dextrose injections—first called “neural prolotherapy,” later Lyftogt named it Perineural Injection Therapy (P.I.T.). While treating chronic tendon problems (for example Achilles tendinopathy), Dr Lyftogt noted that subcutaneous injections around the painful tendon (rather than deep into the tendon itself) produced surprisingly good results — with less pain from the injection and good functional improvement.
- Early case series reported pain reduction in conditions like Achilles tendinopathy, neck pain, headaches, and myofascial pain.
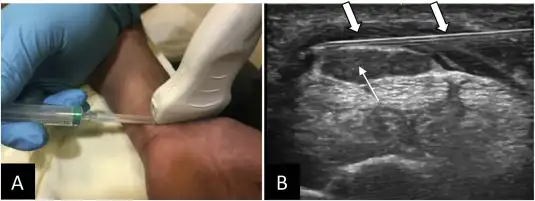
- 2010s–present: Controlled trials emerge, especially for entrapment neuropathies (e.g., carpal tunnel, ulnar neuropathy), and technique papers on ultrasound-guided perineural hydrodissection with D5W.
Proposed mechanisms
The suggested mechanism for Peripheral Nerve Injection Therapy (PIT) involves injecting D5W around painful cutaneous or peripheral nerves. This approach may help reduce TRPV1-mediated hypersensitization, dilute inflammatory mediators, and provide mechanical separation of the nerve (hydrodissection), which could result in reduced pain and enhanced function. Mechanistic reviews, including those from PM&R Now, provide a comprehensive overview of the preclinical rationale.
Safety
Across controlled trials, perineural injections have shown a favorable safety profile (transient soreness/paresthesias are most common.)
3–4 representative studies (high-quality & recent)
- Carpal tunnel syndrome (CTS) — D5W vs. Normal Saline (RCT, double-blind)
Wu YT et al., Mayo Clinic Proceedings 2017
Perineural D5W led to greater pain/disability reduction, improved nerve conduction, and decreased median-nerve CSA vs. saline through follow-up. PubMed+1 (https://pubmed.ncbi.nlm.nih.gov/28778254/)
- CTS — D5W vs. Corticosteroid (RCT, double-blind)
Wu YT et al., Annals of Neurology 2018
D5W produced superior pain and functional improvement compared with triamcinolone at 4–6 months. PubMed(https://pubmed.ncbi.nlm.nih.gov/30187524/)
- Ulnar neuropathy at the elbow (UNE) — D5W vs. Saline (RCT)
Mansiz-Kaplan B et al., Archives of Physical Medicine and Rehabilitation 2022
D5W outperformed saline on pain, disability, motor velocity, and nerve CSA at 4 and 12 weeks. PubMed+1(https://pubmed.ncbi.nlm.nih.gov/35690093/)
- Occipital neuralgia — perineural D5W hydrodissection (case series/technique)
Lam KHS et al., 2024 technique/case report:
Ultrasound-guided greater occipital nerve hydrodissection with 5% dextrose showed promising symptom relief; provides practical positioning and approach details.
- Early clinical findings show that Perineural Injection Therapy can be useful to treat post-concussion symptoms, including pain,
- Early clinical success for foot drop, wrist drop and peripheral nerve injury. Further studies are needed for verification.
Quick takeaways for practice
- Best evidence right now is for entrapment neuropathies (CTS, UNE), where multiple Randomized Controlled Trial’s favor D5W perineural injections over saline and, at intermediate follow-up, over steroids.
- Expanding indications (occipital neuralgia, postsurgical pain, neck pain, headaches, post-concussion syndrome, foot drop, wrist drop, and peripheral injures) have early supportive clinical reports but need further studies.