PRP for Knee Osteoarthritis – Study Shows Favorable Results
Osteoarthritis is a common problem in older adults and is growing into a larger problem – the number of persons experiencing it is increasing. This is alarming because osteoarthritis is hard to treat and traditional therapies have been only partially helpful in reducing symptoms and have not been successful in reversing the damage to joints.
In recent years, efforts to find treatment solutions for a variety of health conditions have explored the use of the patient’s own blood products as a source of growth factors for healing. Currently, orthopedic research studies are examining the effect of platelet-rich plasma (PRP) as a naturally rich source of concentrated growth factors for cartilage repair in persons with osteoarthritis.
An orthopedic medical team from the Rizzoli Orthopedic Institute in Italy conducted a pilot study to test the effect and safety of PRP on joint cartilage. Their findings are summarized here.
The Study Method
- Ninety-one adults with osteoarthritis of the knee were included in the study. A total of 115 knees were treated. Thirty-three knee lesions were classified as early stage lesions and 24 were advanced stage lesions. The average age of participants was 45 years.
- A limiting factor is that no control group was included.
- Evaluations were completed at baseline and were repeated at 2, 6 and 12 months after treatment.
- PRP with a platelet concentration 600% above normal serum levels was given every 21 days for a total of three doses.
- The International Knee Documentation Committee (IKDC) Questionnaire was used to evaluate:
- the patient’s own symptom severity rating
- ability to participate in sports activity
- knee function
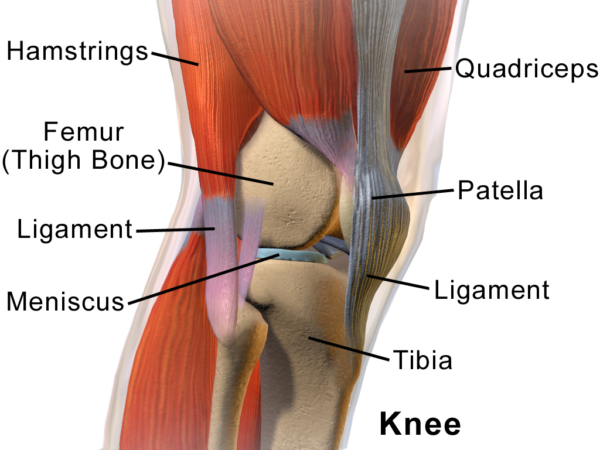
- a physical exam of the knee including; cartilage lesion mapping, ligament status, range of motion, X-ray findings and functional assessment.
Safety Results
- There were no major adverse events.
- In one case there was marked pain and swelling at the injection site. (These symptoms resolved spontaneously in 2 weeks.)
- In some cases there was slight pain at the injection site.
Effectiveness Results
- Significant clinical improvement occurred at 6 & 12 months and 80% of patients were satisfied with treatment.
- The objection, physician-scored portion of the International Knee Documentation Committee Questionnaire increased from 46.1% before treatment to 73% at 6 months and 66.9% at 12 months post treatment.
- Patient’s subjective pain scores improved at 2, 6, and 12 months although there was a tendency for the pain rating to decline somewhat over time.
- Objective scores were lower for patients over age 65 years at every measurement point than for younger patients. Older patients indicated lower effect on pain and subjective scores. This finding is likely related to increased severity of lesions at baseline in older patients. However, 30% of older patients reported significant improvement on subjective scores despite having advanced lesions. Three older patients had unexpectedly good results. The authors’ theory for this effect is that platelets may work at different levels, in other words PRP may contribute to reduced joint inflammation and may reduce the abnormal enlargement of the tissue lining the joint.
- Clinical outcomes were not affected by previous surgery.
- Women and obese persons tended to have less improvement.
Discussion
The positive results of this study are due to the unique activity of growth factors found in blood. You might wonder, “What are growth factors?”
Growth factors are made up of a variety of substances called polypeptides.
A polypeptide is a string of amino acids joined together by a specific chemical bond. These polypeptide growth factors have important roles in determining how cells grow – including the chondrocytes, or joint cells. We now know that many growth factors help regulate joint cartilage. There are different subtypes of growth factors and the subtype that appears to be the most important in cartilage repair is called transforming growth factor-β (TGF-β). TGF- β increases the appearance, development and function of chondrocytes and it stimulates the development of the stem cell line that develops into chondrocytes. Furthermore, TGF-β stimulates growth of cartilage matrix – the supportive “cement” around the chondrocytes, while it dampens many of the destructive effects of inflammatory mediators that impede synthesis of macromolecules needed to build cartilage.
Another polypeptide, called platelet-derived growth factor (PDGF) helps: maintain joint hyaline cartilage, increases the number of chondrocytes, increases the production of specialized joint matrix proteins, and potently draws healing factors into the joint.
Insulin growth factor is important in building cartilage. It may enhance other cartilage-building growth factors as well. There are many other growth factors and they each have some independent effects but together their effects are multiplied beyond their individual effects.
Conclusions
PRP is a concentrated source of growth factors. It is safe, relatively inexpensive, and is minimally invasive. In this pilot study, safety of PRP was demonstrated. There were no infections, no loss of muscle tissue, no incidence of blood clots, no fever, no bruising, or other adverse events. There were minor adverse reactions, mainly mild pain at the injection site that lasted for 2 days, with the exception of 1 case as described above. The average clinical outcome allowed most patients to have a normal daily life experience.
Significant clinical improvement was seen in patients at 6 and 12 months after treatment and 80% of patients were satisfied with treatment. Cartilage lesion mapping, ligament status, range of motion, X-ray findings, functional assessment and pain of the treated knees improved significantly following treatment.
Reference:
Kon, E, Buda, R, Filardo, G, et al. (2009). Platelet-rich plasma: Intra-articular knee injections produced favorable results on degenerative cartilage lesions. Knee Surg Sports Traumatol Arthrosc, DOI: 10.1007/s00167-009-0940-8.
a